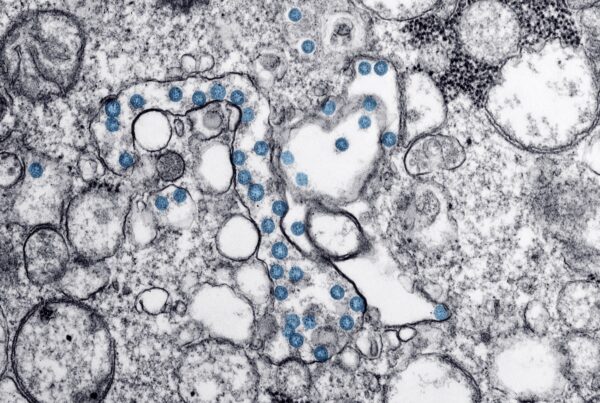
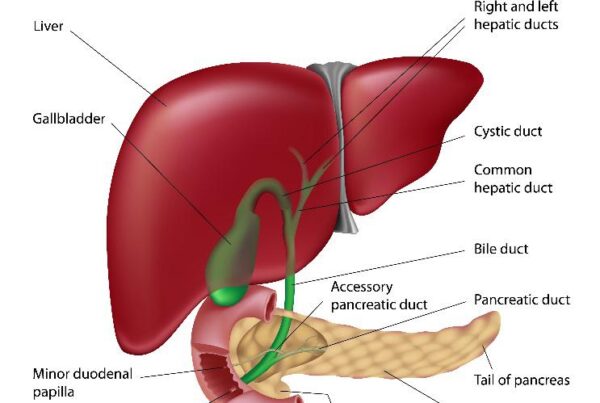
Coronavirus and the GI system: What does the evidence tell us?
August 26, 2020
Coronavirus and the GI system: What does the evidence tell us?
The coronavirus continues to have an enormous impact on the way we live. Over the…



Recent Comments