
Breath Testing
July 15, 2020
Breath Testing
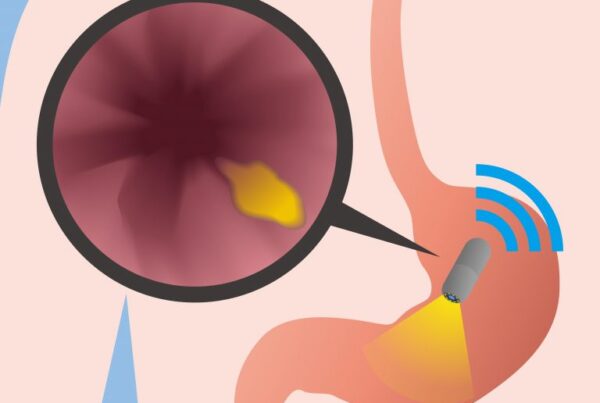
Breath testing is a noninvasive method doctors can use to diagnose gastrointestinal conditions. Here’s what…




Recent Comments