
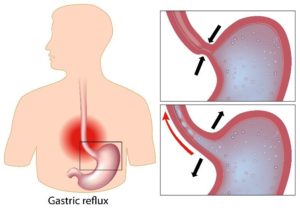
Managing GERD Through Diet: Foods To Seek Out and To Avoid
We’ve all felt it after eating–that burning, uncomfortable feeling in the chest. Maybe you know…




Recent Comments