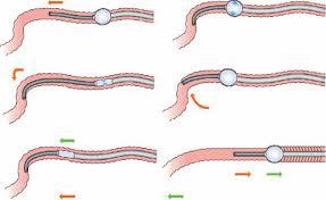
Hemorrhoid Banding: What to Expect
July 22, 2020
Hemorrhoid Banding: What to Expect
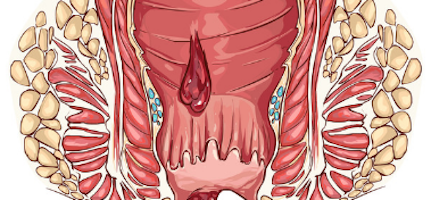
Hemorrhoids are swollen veins in the lower rectum or anus. They can cause bleeding, itching,…



Recent Comments