Radiofrequency Ablation: What You Should Expect
June 24, 2020
Radiofrequency Ablation: What You Should Expect
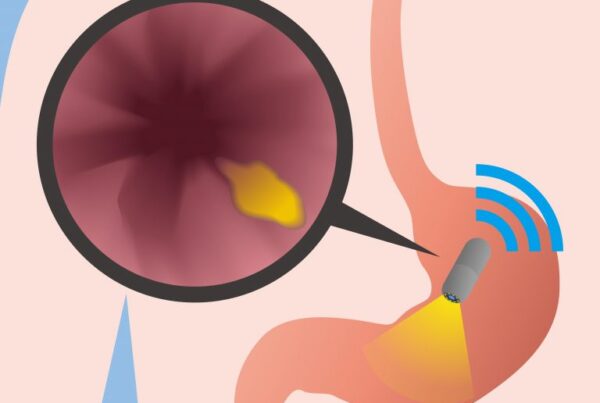
Radiofrequency ablation (RFA) is a procedure that utilizes radio waves to destroy diseased tissue. Here’s…



Recent Comments